Pelvic Organ Prolapse Treatment in Jacksonville, FL
Half of all women develop pelvic organ prolapse, or POP, during their lifetime. And as women are expected to live longer, you can expect to live with POP for a portion of your life.
What is pelvic organ prolapse?
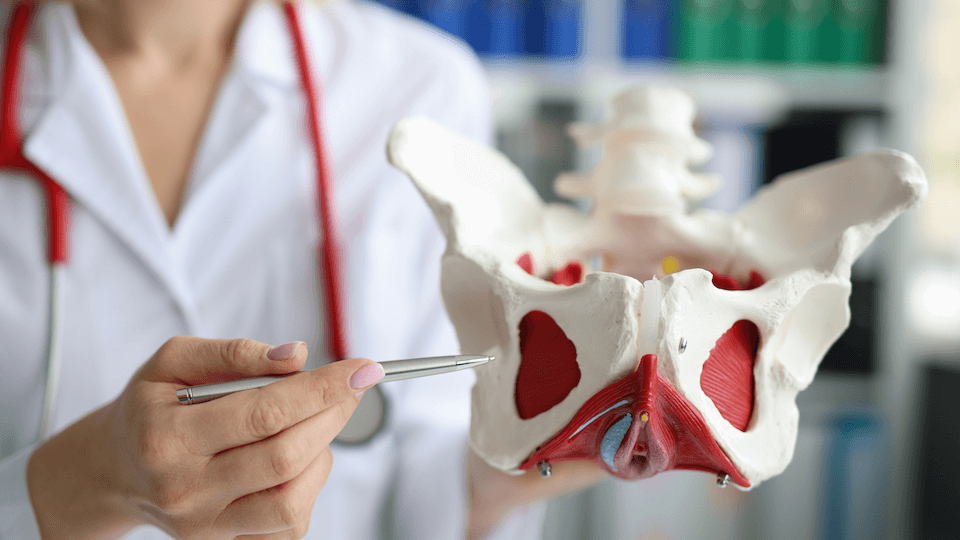
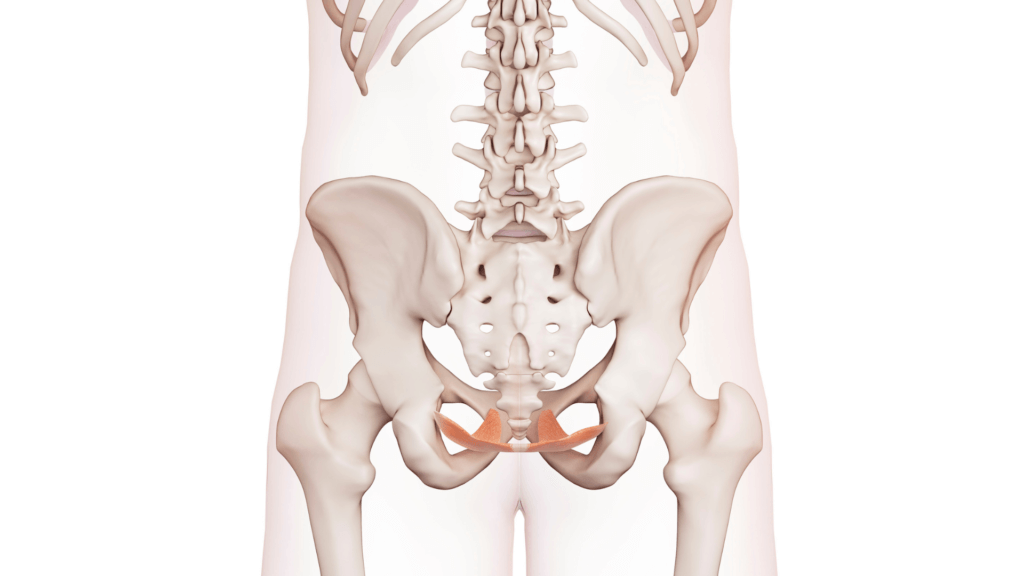
Your pelvic floor is located on the underside of your pelvis. It is a hammock-like support system of muscles, ligaments, and fascia that hold up your pelvic organs. Your pelvic organs are made up of the following:
- Uterus
- Cervix
- Vagina
- Bladder
- Rectum
- Bowels
When the supportive tissues of your pelvic floor fail or weaken, your organs fall and bulge into or outside of your vagina.
When these organs drop from their original positions, you may begin to experience symptoms such as:
- Urinary incontinence
- Overactive bladder
- Fecal incontinence
- Pelvic pain
What does pelvic organ prolapse feel like?
Although your doctor may find a prolapsed organ during your pelvic exam, only 3% of women with POP report symptoms such as pressure, dragging or bulging through their vagina. Some report a ball or lump in their vagina. Others note a lack of sensation during intercourse, painful intercourse, or various urinary and bowel symptoms.
Men can also experience prolapse through their rectum but they report their symptoms less frequently than women.
Where can pelvic organ prolapse occur?
Women have three holes through their pelvic floor where organs can fall out: the urethral canal, vagina, and rectal canal. Most commonly, women experience prolapses through their vaginas. And depending on which organ has fallen, you can experience prolapse from one or multiple locations within your vagina.
A cystocele is the most common type of pelvic organ prolapse. It happens when the bladder or urethra pushes down into the front of your vagina.
The top of the vagina can fall into itself and is called an apical prolapse. It is the second most common type of prolapse and can occur after a hysterectomy.From the back side of your vagina, the rectum can fall down and out, and is referred to as a rectocele.
Common Causes of Pelvic Organ Prolapse
Pregnancy and childbirth are commonly associated with adding excessive pressure onto the pelvic floor, which can cause damage to the nerves, ligaments, and muscles of the pelvic floor. Several factors can increase the risk of pelvic organ prolapse.
- Aging
- Menopause
- Obesity
- Chronic cough
- Chronic constipation
- Heavy lifting
- Disease
Is it serious? And do I have to fix it?
Of those women with pelvic organ prolapse, 40% have mild prolapse or report no symptoms at all. It is considered a non-life-threatening condition, so you can choose to do nothing about it or take action to fix and prevent your prolapse from worsening.
Many women are embarrassed to report symptoms related to their prolapse and will choose to live with it. They may begin to view sexual activity negatively, have a poor sense of their own body image, and experience a decreased quality of life. It’s important to share information regarding unusual symptoms of your pelvic floor with your healthcare provider!
Most POPs are addressed with conservative treatments such as prescribing pessaries or removable devices that are inserted into the vagina to hold organs up. They come in various sizes and shapes to treat prolapse and incontinence.
These vaginal devices can significantly delay or allow you to avoid surgery. They need to be fitted by your healthcare provider. Vaginas come in all sizes and shapes, so they will work with you to help you find the right fit.
Pelvic floor muscle training helps improve your strength to decrease prolapse or prevent it from worsening. It is more successful with milder cases of prolapse. However, there are some cases where training has helped reduce more severe cases.
Treatment Options for Pelvic Organ Prolapse
Avoiding surgery is always preferred, and choosing a conservative approach to treating pelvic organ prolapses is recommended. Exercising and training your pelvic floor muscles have significantly fewer side effects than surgery.
Success in pelvic floor muscle training is highest with younger women and women recovering from recent obstetric trauma. Trauma can include:
- Birthing a child with a high birth weight
- Episiotomy
- Any perineal lacerations during vaginal delivery
And a POP with lesser severity has a higher chance of correcting itself with conservative treatment.
Surgery for Pelvic Organ Prolapse
Surgery is usually the last resort for symptomatic cases. Your surgeon can describe various surgical options and side effects.
Reconstructive surgery restores the positions of your organs and prevents them from falling into your vagina. You can use your body tissues or synthetic mesh to repair and support your organs.
Due to recent safety concerns, a mesh is no longer used to repair prolapse through the vagina but is still used during abdominal repair.
Vaginal closure surgery, or colpocleisis, is used for severe prolapse, which will mean no more intercourse.
Physical Therapy For Pelvic Organ Prolapse
Our physical therapists are specially trained in treating pelvic floor disorders, including pelvic organ prolapse. A pelvic floor therapist will assess and grade the severity of your pelvic organ prolapse based on observing how far the organ has descended down or out of your vagina.
Pelvic organ prolapse is graded using the following stages:
- Stage 0 = no prolapse
- Stage 1 = prolapse is >1 cm from the hymen
- Stage 2 = prolapse is <1 cm from the hymen
- Stage 3 = prolapse is 1-2 cm outside of the vagina
- Stage 4 = the vagina is completely turned inside out
Our pelvic physical therapists are trained to identify and address impairments related to your prolapse and associated pelvic floor issues. They can assess your pelvic floor muscle function around the POP and design a personalized pelvic floor muscle training program.
The purpose is to increase the structural support of your pelvic organs by improving the strength and coordination of your pelvic floor muscles. Your program will include:
- Education and explanation of the function of your pelvic floor’s anatomy and physiology.
- Instructions on contracting and relaxing your pelvic floor muscles with digital palpation, biofeedback, or an electrical stimulation machine.
- Lifestyle and toileting advice to help lessen the load on your pelvic floor and allow for healing and strengthening.
Home exercise program per your physical therapist’s instructions to gain the maximum benefit of training to decrease your symptoms.
